|
|
Precision Orthopaedics and Innovative Technologies (POINT) |
|
Introduction
This theme, Precision Orthopaedics and Innovative Technologies (POINT), consists of different programs:
Laboratory for Orthopaedic Advanced Technology Research
Research Team
 |
 |
 |
Prof. YUNG Shu-hang, Patrick
(ORCID) |
Prof. LAW Sheung-wai |
Prof. WONG Man-yeung, Ronald
(ORCID) |
 |
 |
|
Prof. CHEUNG Wing-hoi, Louis
(ORCID) |
Prof. CHUI Chun-sing, Elvis
(ORCID) |
|
Research Background
Research direction of this team is to develop advanced technology for diagnosis, treatment or prevention of orthopaedic diseases. Artificial intelligence (AI), robotics, augmented reality (AR) will be applied to develop cutting-edge devices or facilities targeting to facilitate early diagnosis, improved and more precise surgery procedures or treatment, as well as effective prevention of various orthopaedic diseases, which would ultimately achieve precision medicine. This team is composed of multidisciplinary experts, including orthopaedic surgeons, biomedical engineers and scientists to collectively develop advanced technologies to solve orthopaedic problems. This joint force expects to translate their research work into products to benefit patients suffering from musculoskeletal disorders and to achieve healthy ageing for the senior citizens.
Research Direction
| • |
Development of AI-based platforms for diagnosis and surgery of musculoskeletal diseases |
| • |
Development of robotics and augmented reality to facilitate medical education and orthopaedic surgeries |
| • |
Application of developed advanced 3D technologies in orthopaedics |
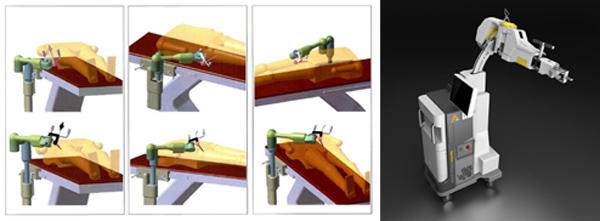
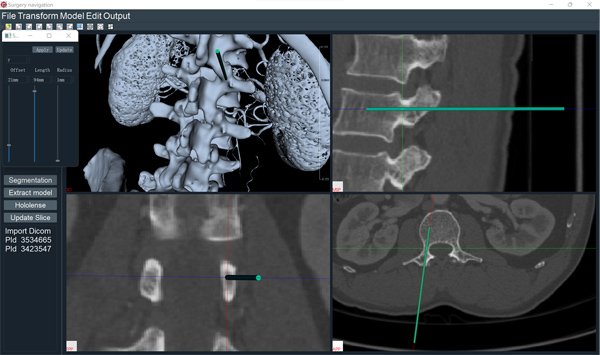
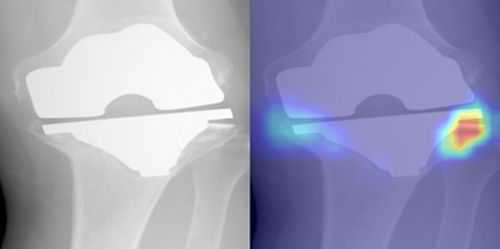
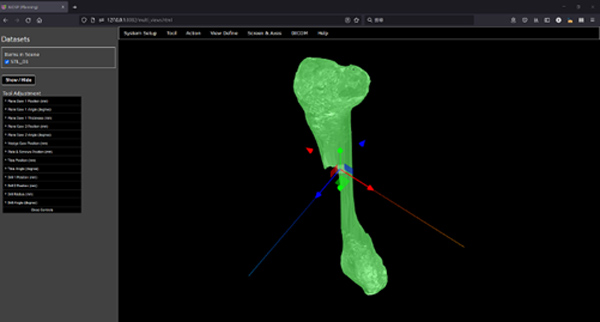
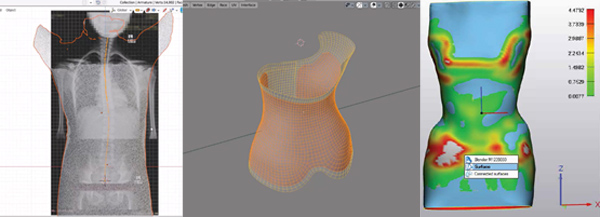
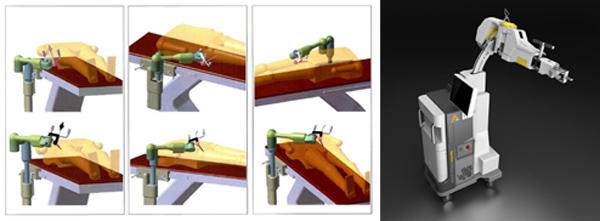 Fig 1. Passive active robot for orthopaedic surgery HybriDot  Fig 2. AR assisted pedical screw insertion module for orthopaedic surgery training 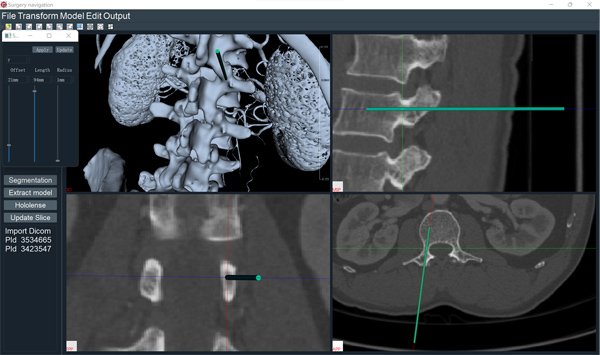 Fig 3. Intra-operative planning - AR navigation system 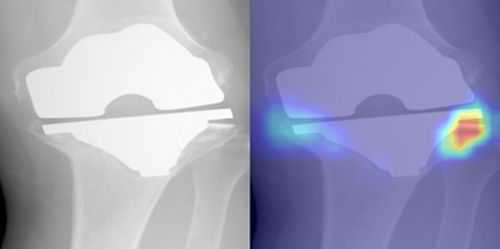 Fig 4. Deep learning based prosthesis loosening detection 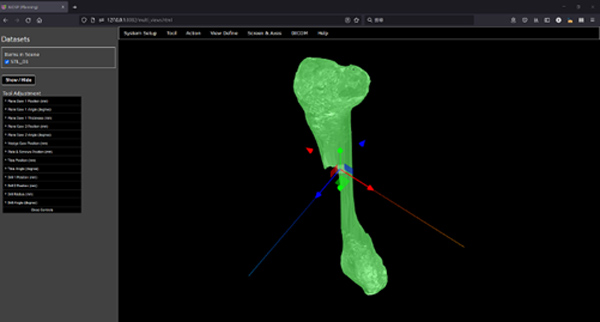 Fig 5. Artificial intelligence assisted orthopaedic surgery planning system 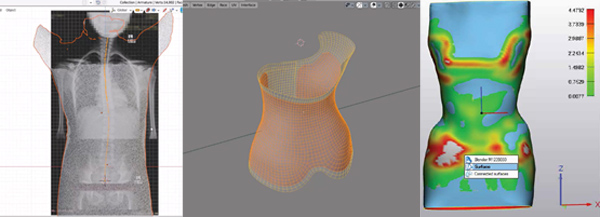 Fig 6. Semi-automatic 3D spine bracing designing system
Current On-going Projects
|
Project Titles |
| 1. |
Artificial intelligence assisted orthopaedic surgery planning system |
| 2. |
AR navigated orthopaedic surgical robot arm (ARTHOR) and AI-assisted 3D surgery planning system (ARTHORPLAN) |
| 3. |
Application of machine learning models in hospital stay prediction for fragility fracture |
| 4. |
Artificial intelligence assisted osteoporosis detection system |
| 5. |
Artificial intelligence assisted orthopaedic prosthesis design and surgical planning system |
| 6. |
Deep learning and CT based automatic segmentation algorithm and software system for human anatomy |
| 7. |
Augmented reality in orthopaedic trauma |
| 8. |
Deep learning-based scoliosis progression prediction model based on multiple imaging modalities |
| 9. |
Joint replacement prosthesis loosening detection |
| 10. |
Artificial intelligence assisted vertebral fracture detection system |
Completed Projects
|
Project Titles |
Funding Agency |
Awarded Year |
| 1. |
Computerized semi-automatic system for surgical planning and patient specific instrument design for corrective osteotomy |
Koln 3D Technology (Medical) Limited |
2018 |
| 2. |
Development of population based total knee replacement prosthesis for Chinese |
Innovation and Technology Fund |
2017 |
| 3. |
3D-printed Surgical Instruments and Orbital Models (3SIOM) |
Innovation and Technology Fund |
2016 |
| 4. |
Effect of Lattice Size in Metallic Orthopaedic Implants on Bone In-growth |
Shandong Weigao Orthopaedic Device Co., Ltd |
2013 |
| 5. |
Development and manufacturing of semi-active surgical robot arm system for computer assisted orthopaedic surgery (CAOS) |
Innovation and Technology Fund |
2011 |
Patents
| Title |
Country |
Status |
| Surgical robot with hybrid passive/active control |
USA
China |
US 8,961,537 B2
L201210307007.9 |
| Method for producing knee replacement implant and implant for knee replacement |
USA
China |
US 10,357,369 B2
ZL01710116367.3 |
| Semi-automated imaging reconstruction for orbital fracture repair |
USA |
US2020261231A1 |
| Rigid surgical stent |
HK |
WO2020044128A1 |
| 一種基於AR的根管監測方法及系統 |
China |
CN110269715B |
Awards
| Awards |
Project title |
Event |
| Gold Medal |
Ultrasound-Based Navigation System for Minimally Invasive Fracture Reduction |
49th International Exhibition of Inventions of Geneva 2024 |
| Gold Medal |
Automated Patient-Specific Prosthesis Design System for Bone Defects |
| Gold Medal |
Deep Learning Method and System for Bone Health Status Evaluation and Osteoporosis Diagnosis |
| Gold Medal |
Semi-automatic 3D Planning Software for Osteotomy Jig Generation |
48th International Exhibition of Inventions of Geneva 2023 |
| Bronze Medal |
Machine Learning Algorithm for Knee Arthroplasty Loosening Detection |
| Bronze Medal |
Semi-Automated Imaging Reconstruction for Orbital Fracture Repair |
 Fig 7. Certificates from the 48th International Exhibition of Inventions of Geneva in 2023.
Selected Publications
| 1. |
Chui CS, Lau CML, Ye X, Hung LH, Kwok KB, Chow KH, Yeung RMY, Cheung WH, Yung PSH. Improving the performance of V-net architecture for volumetric medical image segmentation by implementing a gradient pre-processor. Clin Surg. 6:3383, 2021. |
| 2. |
Wong RMY, Wong PY, Liu C, Chung YL, Wong KC, Tso CY, Chow SK, Cheung WH, Yung PS, Chui CS, Law SW. 3D printing in orthopaedic surgery: a scoping review of randomized controlled trials. Bone Joint Res. 10(12):807-19, 2021. |
| 3. |
Chui CS, Leung KS, Qin JH, Shi DF, Augat P, Wong RMY, Chow SKH, Huang XY, Chen CY, Lai YX, Yung PSH, Qin L, Cheung WH. Population-based and personalized design of total knee replacement prosthesis for additive manufacturing based on Chinese anthropometric data. Engineering. 7(3):386-94, 2021. |
| 4. |
Chui CS, Lau LCM, Kwok CKB, Ng JP, Hung YK, Yung PSH, Fan JCH. Tibial cutting guide (resector) holding pins position and subsequent risks of periprosthetic fracture in unicompartmental knee arthroplasty: a finite element analysis study. Journal of Orthopaedic Surgery and Research 2021 March, 16 (1) |
| 5. |
Chui CS, Kwok KB, Mak KK, Yung PSH, Lau LCM. Novel Application of 3D Printing to Development of a Homemade Posterior-Stabilized Knee Cement Spacer. Clin Surg. 2021;6(1):3385 |
| 6. |
Lau LCM, Chui ECS, Fan JCH, Man GCW, Hung YW, Ho KKW, Chung KY, Wan SYC, Chau WW, Yung PSH, Bhandari M. Patient Specific Instrumentation (PSI) Referencing High Tibial Osteotomy Technological Transfer and Education: Protocol for a Double-blind, Randomized Controlled Trial (PROTECTED HTO Trial). BMJ Open 2021 February, 11 (2) |
| 7. |
Chim YN, Chow SKH, Mak SY, Li MMC, Yung BCH, Yau EWF, Chui CS. 3D-printed cobalt-chromium porous metal implants showed enhanced bone-implant interface and bone in-growth in a rabbit epiphyseal bone defect model. Bone Reports 2020 October, 13:100375 |
| 8. |
Fang C, Cai H, Kuong E, Chui CS, Siu YC, Ji T, Igor D. Surgical applications of three-dimensional printing in the pelvis and acetabulum: from models and tools to implants. Der Unfallchirurg 2019 March, 122 (4) |
| 9. |
Qin LY, Wen JZ, Chui CS, Leung KS. Housing design and testing of a surgical robot developed for orthopaedic surgery. J Orthop Translat. 5:72-80, 2016. |
| 10. |
Liu W, Kuang S, Wang Y, Chui CS, Leung KS, Fan Y. Interactive Path Planning for 2D Fluoroscopy-based Orthopaedic Navigation. IFMBE proceedings. 2013 January, 39: 2138-2141. |
| 11. |
Wang Y, Kuang S, Liu W, Chui CS, Leung KS, Fan YB. The DEA-based Efficiency Evaluation of HybriDot: An Active-Passive Hybrid Surgical Robot for Orthopaedic Surgery. IFMBE proceedings. 2013 January, 39:2174-2177. |
| 12. |
Kuang S, Leung KS, Wang T, Hu L, Chui CS, Liu WY, Wang Y. A novel passive/active hybrid robot for orthopaedic trauma surgery. International Journal of Medical Robotics and Computer Assisted Surgery. 2012 December, 8 (4) |
Innovative Orthopaedic Biomaterial and Drug Translational Research
Research Team
Program Director |
Program Co-Directors |
 |
 |
 |
Prof. QIN Ling
(ORCID) |
Dr. TANG Ning |
Prof. YUNG Shu-hang, Patrick
(ORCID) |
 Team Members (Photo taken in Jan 2025)
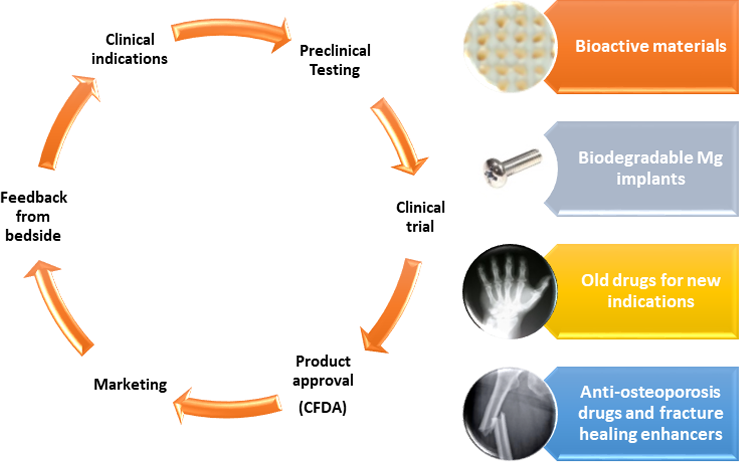
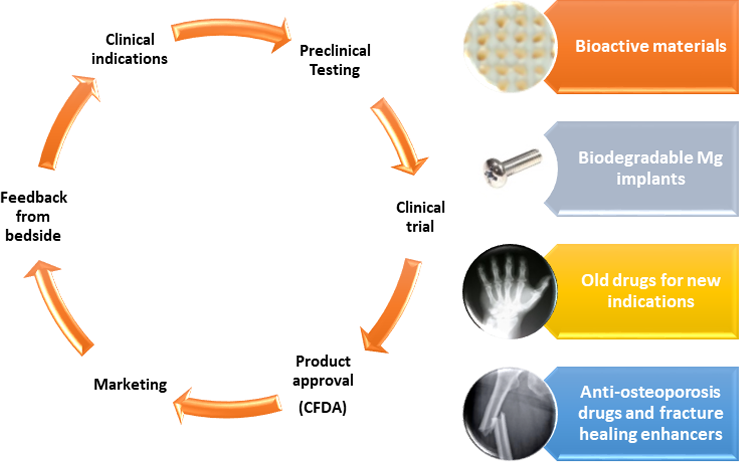 Overview of our roadmap for translational research, from establishing clinical indications to preclinical assessments, clinical trials, regulatory approval, and realization of our research outcome in clinical applications of our Class III medical implants, devices, and drugs
Research Background
Population aging is a global challenge. Ageing is associated with many musculoskeletal problems, including primary or secondary osteoporosis (OP), osteoarthritis (OA), and chronic tendon-bone insertion (TBI) disorder or injury, which often lead to bone fractures, joint deformity, and disability. These costs impose a huge socioeconomic and healthcare burden on the patient, family, healthcare system, and society in Hong Kong and worldwide. Therefore, there is an urgent need for further development or improvement of orthopaedic implants/devices, drugs/supplements to prevent or treat musculoskeletal disorders, and accelerate musculoskeletal regeneration. The World Health Organization (WHO) designated 2000-2010 as the Bone Joint Decade and has subsequently extended it to 2020, which implies musculoskeletal diseases are a big challenge for our modern yet aging society.
Our research focuses on the development of orthopaedic implants/devices with innovative biomaterial or hybrid systems and medical drugs/nutrition supplements for orthopaedic diseases or injuries, such as osteoporosis, osteoporotic fractures, and osteonecrosis. By integrating medical science, life science, material science, pharmacological science, imaging technology, and biomechanics, we identify potential solutions for clinical problems. Then, we collaborate with our industrial partner to transform our research into medical products that benefit patients. The feedback from patients and clinicians would refine future R&D and improve the quality of innovative products.
Research Directions
| • |
Biodegradable and bioactive metallic orthopaedic implants |
| • |
Osteopromotive agents for the treatment of osteoporosis and osteonecrosis |
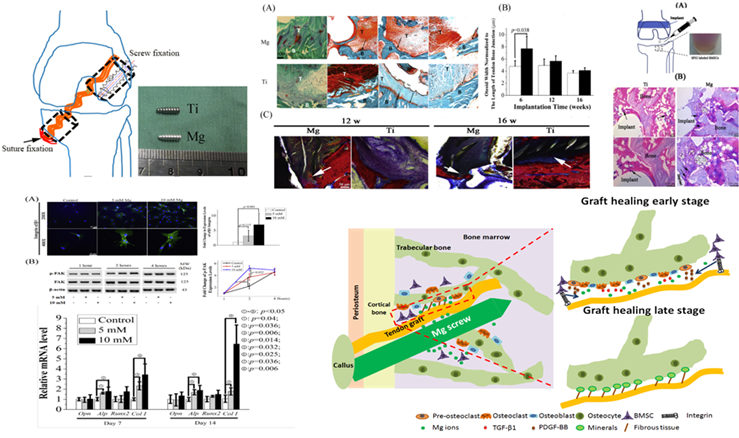
Biodegradable and Bioactive Metallic Orthopaedic Implants
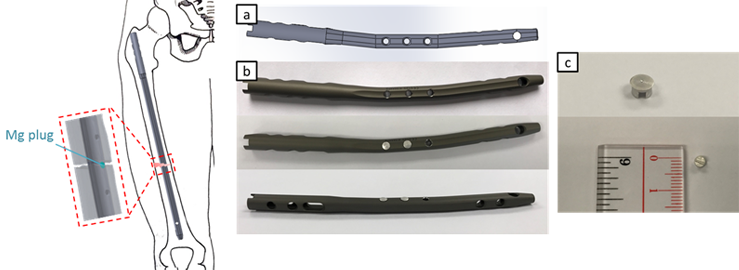
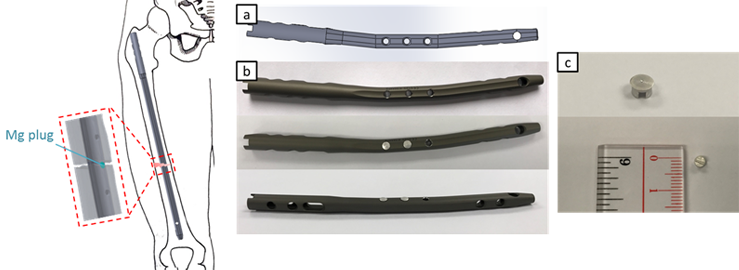 Fig 1.1. Hybrid implant for fracture fixation. Schematic diagram of the hybrid system after surgery. The Mg plug is close to the fracture site. The released Mg ions would be distributed to the surrounding tissue and promote fracture healing. (a) CAD model of modified IM nail; (b) The prototype of the hybrid IM nailing system with insertion of Mg plug; (c) The fabricated Mg plug.
Our innovative and patented biodegradable implants made of pure magnesium (Mg) or its alloys have demonstrated initial stable fixation ability and regeneration in challenging orthopaedic conditions, including treatment of osteoporotic fractures, osteonecrosis, and bone-tendon insertion (TBI) repair. Our collaborators from both academia and industry provide platforms for realizing our proof-of-concept implants for our collective efforts in clinical translation and bedside applications. Our preclinical and clinical research and published work serve as key references for regulatory bodies, such as the US FDA and Chinese FDA, for establishing ISO standards and guidelines for developing biodegradable metallic implants.
Professor Ling Qin focuses on the R&D of innovative orthopaedic implants and drugs or supplements for the prevention and treatment of skeletal disorders and injuries with limited healing potential, including patients with impaired healing capacity, large bone defects, and healing at different tissue types such as the bone-tendon/bone-cartilage interface. He has been developing innovative biomedical and tissue engineering products, clinical indication-oriented treatment regimens and protocols that utilize stem cells, bioactive and biodegradable materials (e.g., biodegradable Magnesium), endogenous and exogenous growth factors, and external biophysical stimuli to enhance musculoskeletal tissue regeneration. The goal of his research is to facilitate not only anatomical but more importantly also functional restoration to achieve early rehabilitation and reduce disease-associated morbidity and mortality.
Being multidisciplinary in nature, Professor Qin and his team collaborate with local and international engineers and material scientists for developing innovative biomaterials and drugs, such as redesigning the current commercially available implant to incorporate Mg-based components. Recently, we have tested different Mg-based alloys and have applied different coatings to prevent the rapid degradation. One innovative approach is that we have modified current commercially available implants to incorporate Mg-based components to enhance bone healing. This hybrid implant, with both conventional titanium metal and Mg components, can deliver Mg to fracture sites and also has great potential in facilitating and enhancing fracture healing, which could accelerate an early initiation of mobility and rehabilitation of patients with fractures.
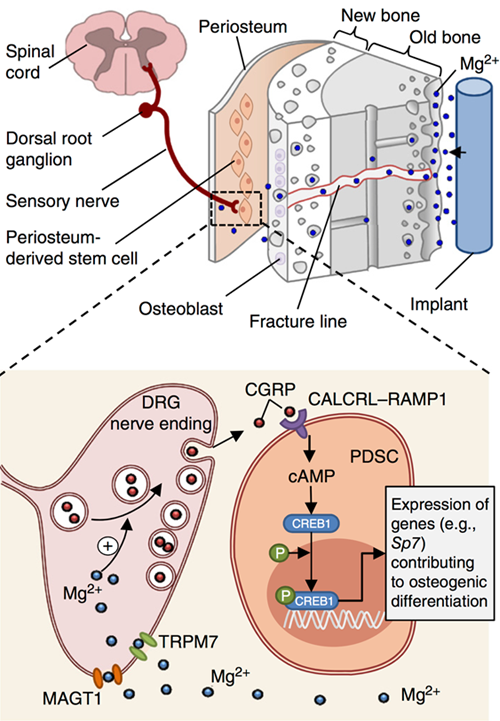
Recently, with collective efforts and endeavors, Professor Qin's R&D program has secured significant R&D and scientific competitive grants, including the Areas of Excellence Scheme (AoE/M-402/20), Theme-based Research Scheme (T13-402/17-N), and Collaborative Research Fund (C4028-14G, C4026-17W), which are three of the most competitive grants schemes given by the Research Grant Council of the Hong Kong Special Administrative Region. Our team in CUHK has been dedicating our efforts to innovation and R&D of the biodegradable magnesium (Mg)-based implants to develop desirable novel medical implants for avoiding or overcoming the above-mentioned drawbacks. Moreover, as shown in our recent Nature Medicine and Materials Today articles, to promote fracture healing and bone regeneration via the special osteo-promotive property of the Mg implants, which are partially through the nerve system and the calcitonin gene-related peptide (CGRP) in the challenging osteoporotic and bisphosphonate-associated atypical femoral fractures. Our innovative R&D has also received global attention, including an Innovation feature or Research Highlights by Nature in 2018 and Science in 2022. We have successfully designed and developed many novel Mg-based implants for a number of orthopaedic indications, including various fractures and bone defects at different skeletal sites, as well as anterior cruciate ligament (ACL) reconstruction, protected with the USA and PRC patents and recognized with Geneva Invention awards. We verified their function and efficacy by using the well-established animal models and disclosed the mechanism via the cellular and molecular experiments, especially the cutting-edge single-cell sequencing and analysis platform to identify the key genes responsible for the effect of the biodegradable Mg-based implants that lay down a solid foundation for designing our biodegradable implants to facilitate and accelerate bone regeneration and fracture healing.
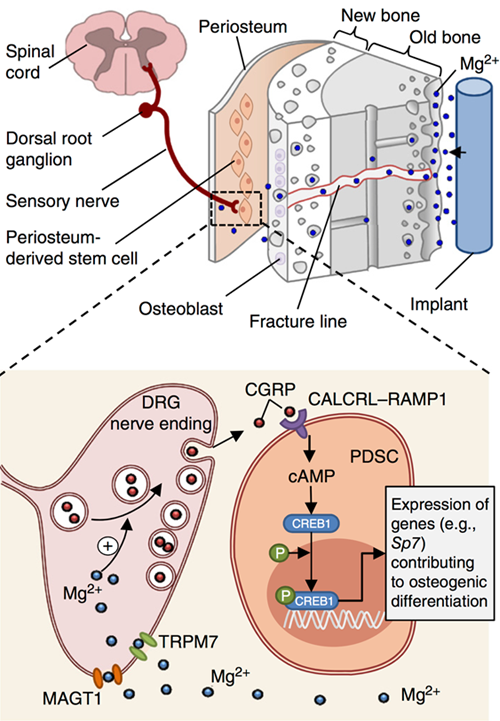 Fig 1.2. Schematic diagram showing diffusion of implant-derived Mg2+ across the bone toward the periosteum that is innervated by DRG sensory neurons and enriched with PDSCs undergoing osteogenic differentiation into new bone (top). Inset (shown enlarged at bottom), the released Mg2+ enters DRG neurons via Mg2+ transporters or channels (i.e., MAGT1 and TRPM7) and promotes CGRP-vesicles accumulation and exocytosis. The DRG-released CGRP, in turn, activates the CGRP receptor (consisting of CALCRL and RAMP1) in PDSCs, which triggers phosphorylation of CREB1 via cAMP and promotes the expression of genes contributing to osteogenic differentiation. [Zhang Y et al., Nat Med. 2016 Oct;22(10):1160–9.]
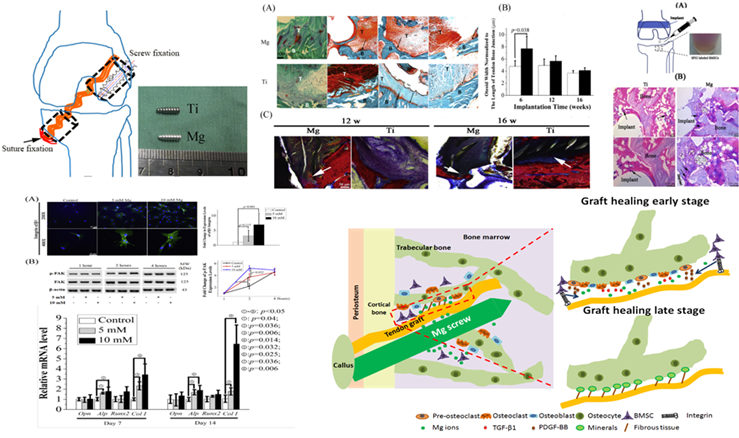
Fig 1.3. Mg-based interference screws can promote the formation of the mineralized fibrous tissue at the tendon-bone interface via increasing the migration ability, adhesion capability, and osteogenic differentiation potential of bone marrow stem cells [Wang J et al. Acta Biomater. 2017 Nov;63:393–410.]
Osteopromotive Agents for the Treatment of Osteoporosis and Osteonecrosis
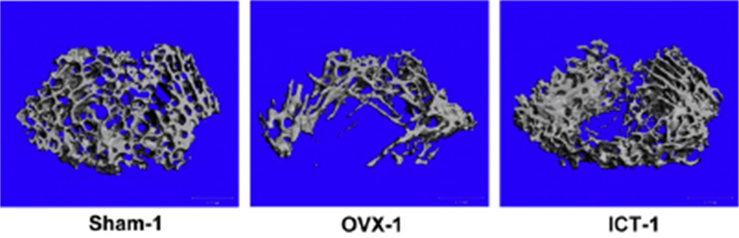
Icaritin, a phytoestrogen with a similar function and structure to estrogen, is extracted from the Epidemii herb. Our previous studies demonstrated the beneficial effect of icaritin on osteoporotic bone in both animals and humans.
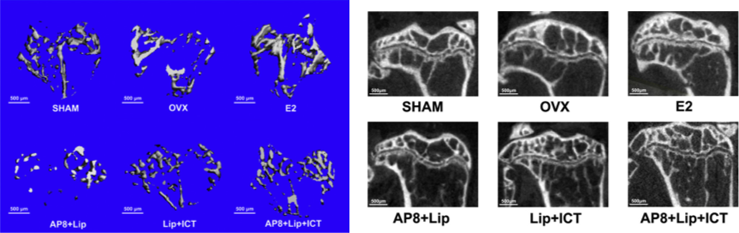
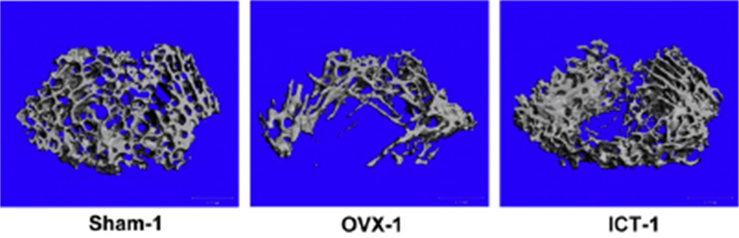 Fig 2.1. 3D micro-CT image of trabecular bone in proximal tibia of mice. Mice with ovariectomy (OVX) were established as an osteoporotic model (OVX-1). Icaritin was given as treatment one month after surgery (ICT-1).
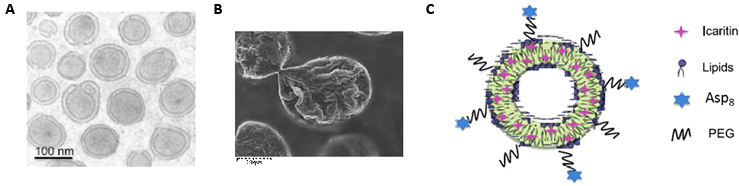
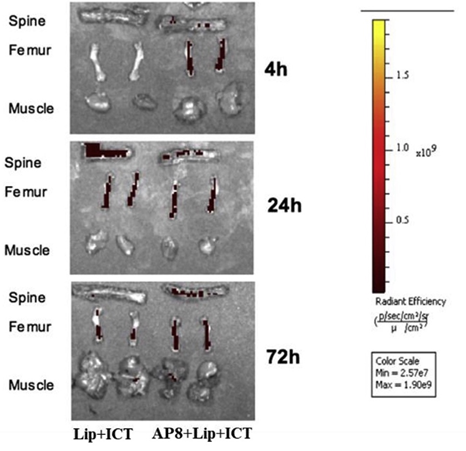
Since the oral bioavailability of icaritin is low (around 10%-17% reported by previous studies) and the retention time in blood circulation is relatively short, a bone-targeting liposome delivery system was developed. This delivery system has been reported in our previous study published in Nature Medicine and Biomaterials (Zhang G et al. Nat Med. 2012 Feb;18(2):307–14; Huang L et al. Biomaterials. 2018 Nov;182:58–71.).
| • |
Liposome. Its stability can lead to a long circulation time after intravenous administration. |
| • |
Asp 8. Stronger affinity to the bone-resorption surface characterized by highly crystallized hydroxyapatite. |
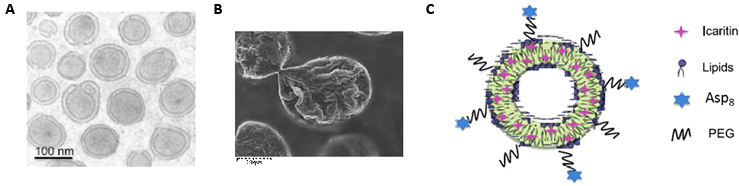 Fig 2.2 The targeting delivery system with icaritin. A: The bilayer liposome structure under TEM. B: Icaritin delivery system under SEM. C: Schematic diagram of our bone-targeting delivery system
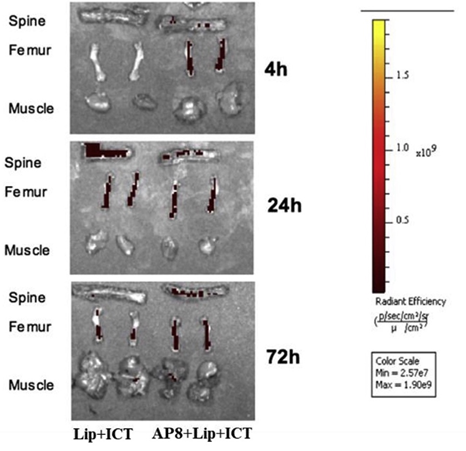 Fig 2.3. Tissue distribution after labeled liposome-icaritin and (Asp)8-liposome-icaritin ex vivo. A fluorescence-labeled delivery system with or without a targeting peptide was injected into mice. Organs have been harvested at different time points and scanned with an IVIS fluorescence detector.
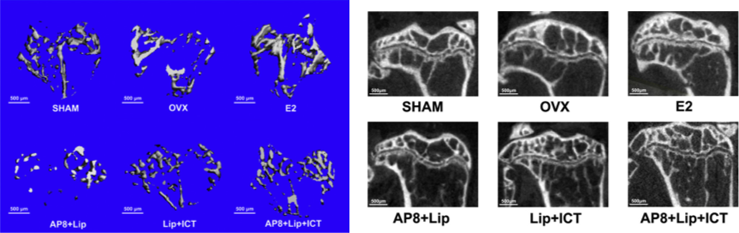 Fig 2.4. Icaritin in the bone-targeting delivery system prevents bone loss in OVX mice. Ex vivo micro-CT quantification of the bone mineral density (BMD) and 3D trabecular architecture at proximal tibia in groups with or without ovariectomy surgery (OVX) and treated with administration of different treatments including oral administration of estradiol (E2) and intravenous injection of targeting delivery system (AP8+Lip), delivery system with icaritin (Lip+ICT) and targeting delivery system with icaritin (AP8+Lip+ICT).
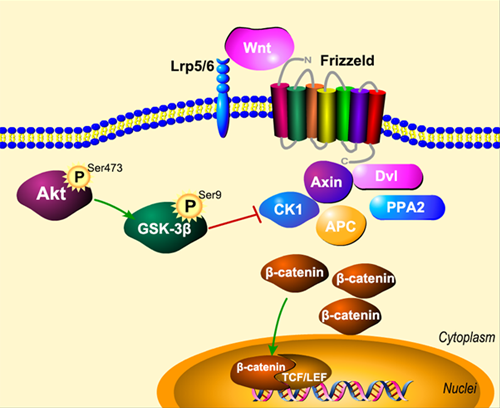
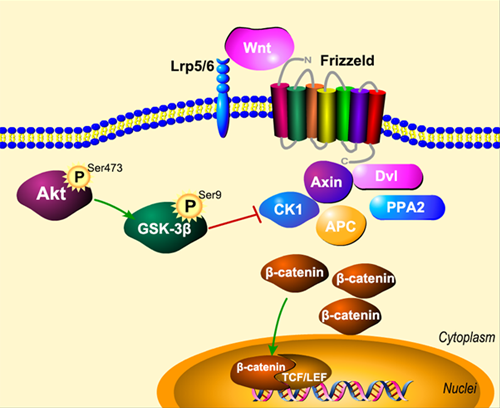 Fig 2.5. Icaritin regulates adipogenesis through the Akt-GSK-3β/β-catenin signaling pathway. Icaritin promotes the phosphorylation of Akt, and phosphorylated Akt can further phosphorylate GSK-3β, thus inhibiting the combination of the β-catenin destruction complex. Therefore, β-catenin accumulates in the cytoplasm and then transfers into nuclei to activate the downstream of β-catenin signaling pathway to further promote osteogenesis and inhibit adipogenesis of BMSCs.
Research Impacts
Patents
| Title |
Applicants |
Status |
Reference Number |
| 骨植入物 |
秦岭、谢鑫荟、郑玉峰 |
授权公告日
(2013.12.11) |
中华人民共和国国家知识产权局
ZL2013 2 0005009.2 |
| 骨固定组件及其用途 |
秦岭, 田立, 魏涛, 吴奇, 梁国穗 |
授权公告日
(2017.09.05) |
中华人民共和国国家知识产权局
CN 104906638 B |
| Hybrid Implant system and manufacturing method therefor |
Ling Qin, Yeu Sun Cheng, Ning Tang, Wing Ho Chau |
Date of Patent:
(2020.01.07) |
United States Patent
US 10,525,173 B2 |
| 内植物混合系统及制造方法 |
秦岭, 郑玉臣, 邓宁, 周泳豪 |
授权公告日
(2022.05.10) |
中华人民共和国国家知识产权局2
CN 108309421 B |
| 骨植入物 |
秦岭,祖海越,许建坤,黄文扬,赵德伟 |
授权公告日
(2024.03.19) |
中华人民共和国国家知识产权局
CN 115252229 B |
 Fig 3.1 Patents certificates.
Awards
| • |
Gold Medal, 15th International Invention Fair in the Middle East |
| • |
Gold Medal, 13th International Invention Fair in the Middle East |
| • |
Gold Medal with the Congratulations of the Jury, 46th International Exhibition of Inventions of Geneva 2018 |
 Fig 3.2. Certificates from the International Exhibition of Inventions.
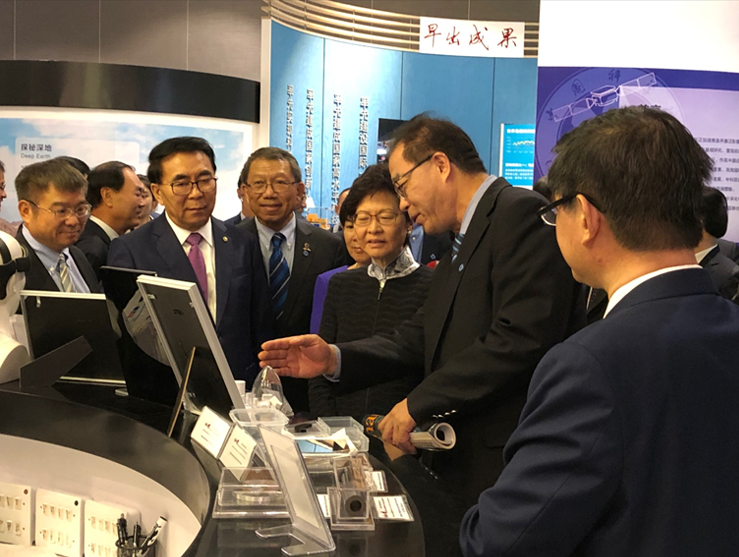
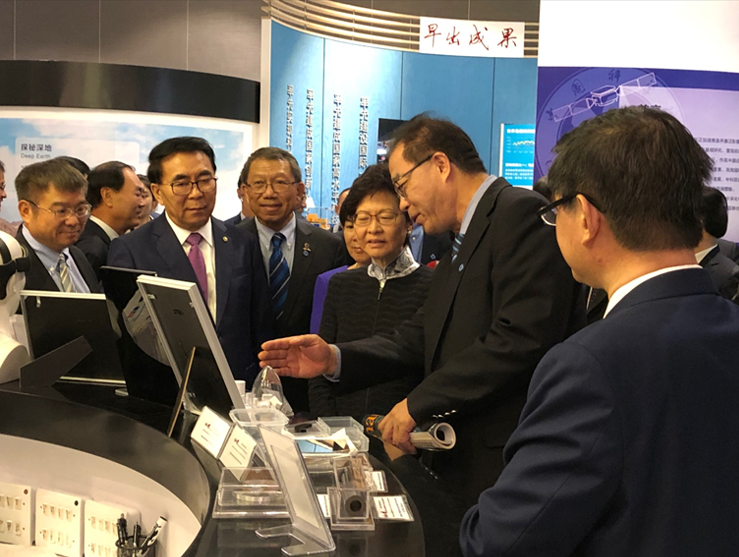 Fig 3.3. Program director Professor Ling QIN (2nd from right) was showing Ms. Carrie LAM (Previous Chief Executive of Hong Kong, 3rd from right) Professor Rocky TUAN (Previous Vice Chancellor of CUHK, 3rd from the left) and Professor Chunli BAI (Previous President of the Chinese Academy of Sciences, 2nd from left) the innovative biodegradable Magnesium-based orthopaedic implants (Nov 8, 2018).
10 Selected and Representative Publications from a Total of over 500 SCI Papers
| 1. |
Shao H, Xu S, Zeng F, Jin Z, Ji X, Shan Z, Kang J, Tian Q, Zhang S, Mao Z, Zhang Y, Xu J, Tong W*, Qin L*. Metal-Organic Framework-Integrated Nanoplatform Orchestrates Osteochondral-Synovial Homeostasis for Osteoarthritis Therapy. ACS Nano, 2025 Sep 16;19(36):32744-32766. |
| 2. |
Li X, Liang T, Dai B, Chang L, Zhang Y, Hu S, Guo J, Xu S, Zheng L, Yao H, Lian H, Nie Y, Li Y, He X, Yao Z, Tong W, Wang X, Chow DHK, Xu J, Qin L*. Excess glucocorticoids inhibit murine bone turnover via modulating the immunometabolism of the skeletal microenvironment. The Journal of Clinical Investigation, 2024 Mar 21;134(10):e166795. |
| 3. |
Zu H, Zheng L, Huo M, Liu K, Zhang Y, Shi K, Cao H, Zu X, Tong W, Xu J, Ding M, Lu J, Qin L*. (2024). Tree-inspired Magnesium Hybrid Column for Preventing Hip Collapse in Steroid-associated Osteonecrosis in Bipedal Emus. Materials Today, Sept 2024. Online. |
| 4. |
Dai B, Xu J, Li X, Huang L, Hopkins C, Wang H, Yao H, Mi J, Zheng L, Wang J, Tong W, Chow DH, Li Y, He X, Hu P, Chen Z, Zu H, Li Y, Yao Y, Jiang Q, Qin L. Macrophages in epididymal adipose tissue secrete osteopontin to regulate bone homeostasis. Nature Communications, 2022 Jan 20;13(1):427 |
| 5. |
Zheng N, Xu J, Ruan Y, Chang L, Wang X, Yao H, Tang N, Ong T, Schilcher J, O’Keefe R*, Qin L*. Magnesium facilitates the healing of atypical femoral fractures: A single-cell transcriptomic study. Materials Today, Vol 52, January–February 2022, Pages 43-62. |
| 6. |
Chow DHK, Ong MTY, Tong W, Qin L*. Biodegradable magnesium pins enhanced the healing of transverse patellar fracture in rabbits. Bioactive Materials, 27;6(11), 2021. |
| 7. |
Tian L, Sheng Y, Chow DH, Tang N, Ngai T, Lu J, Qin L*. An innovative Mg/Ti hybrid fixation system developed for fracture fixation and healing enhancement at load-bearing skeletal site. Biomaterials, 180:173, 2018. |
| 8. |
Wang J, Xu J, Song B, Shu-Hang Yung P, Qin L*. Magnesium (Mg) based interference screws developed for promoting tendon graft incorporation in bone tunnel in rabbits.Acta Biomaterialia. 2017 Nov;63:393-410. |
| 9. |
Zhang YF, Xu JK, Ruan YC, Chow DH, Huang S, KS Leung, Lu N, Zhao DW, Zheng YF, Qin L*. Implant-derived magnesium induces local neuronal production of CGRP to promote bone fracture healing in rats. Nature Medicine, 22(10):1160-1169, 2016 |
| 10. |
Zhao D*, Huang S, Lu F, Wang B, Yang L, Qin L*, Li W, Wang W, Tian S, Zhang Y, Xie X, Wang J, Li J. Vascularized bone grafting fixed by biodegradable magnesium screw for treating osteonecrosis of the femoral head. Biomaterials, 81:84-92. 2016 |
 Prof. Qin’s team has focused on the discovery of innovative biomaterials with a focus on R&D of Mg-based medical implants for 15 years, with fruitful outputs. There are 10528 academic publications in Web of Science with the topic Mg for Bone from January 2015 to March 2025, and according to the citation numbers, 5 of the top 10 are from Prof. Qin’s team (No. 1, 2, 3, 4, and 10). This indicates the profound international recognition of academic achievements.
Funding Support (recent 5 years)
| Project Title |
Duration |
Grant-giving Body |
Funded Amount (HKD$) |
| No pain no gain in skeletal regeneration? |
2025.1-2026.12 |
RGC-GRF |
1,600,000 |
| Translation of Magnesium-Based Biodegradable Implants as Innovative Class III Medical Devices for Clinical Use: Pre-Clinical Activities and Commercialization Plan |
2024.4-2028.3 |
CUHK, Faculty of Medicine |
1,600,000 |
| Magnesium-Based Biodegradable Implants as Innovative Class III Medical Devices: From Implant Design, Biosafety, Efficacy to Clinical Translation |
2024.4-2028.3 |
RGC-RIF |
4,000,000 |
| Aging, Skeletal Degeneration and Regeneration |
2021.5-2029.4 |
RGC-AoE |
70,688,000 |
| Prevention and treatment of osteoarthritis by screening a novel cartilage-targeting adeno-associated virus: a gene therapy approach |
2022.7-2025.6 |
HMRF |
1,425,000 |
| Magnesium Activated Progenitor Cells in Synovial Fluid to Regenerate Articular Cartilage |
2022.1-2024.12 |
RGC-GRF |
1,174,000 |
| Differential Roles of CGRP in Osteoarthritis Pain and Pathology |
2022.1-2025.12 |
NSFC-RGC |
1,185,600 |
| An Innovative Strategy Recapitulates the Neuropeptide-Guided Angiogenic-Osteogenic Coupling for Functional Repair of Segmental Bone Defect |
2022.1-2023.12 |
RGC-GRF |
1,175,000 |
| Multifunctional Bioactive 3D-Printed Scaffold as an All-in-One Platform for Postsurgical Osteosarcoma Treatment and Bone Defect Repair |
2021.11-2023.10 |
ITC |
1,900,000 |
| Fibroblasts as a Novel Therapeutic Target for Enhancing the Healing of Challenging Bone Fracture |
2021.6-2024.5 |
HMRF |
1,500,000 |
| Identification of a Central to Sympathetic Neural Circuit in Magnesium-promoted Bone Regeneration using Retrograde Tracing and Single-cell RNA-seq |
2021.1-2023.12 |
RGC-GRF |
1,126,000 |
| Functional Bone Regeneration in Challenging Bone Disorders and Defects |
2017.11-2023.6 |
RGC-TRS |
33,333,000 |
Bone Tumor Team
Introduction
The Bone Tumor Team in the Department of Orthopaedics and Traumatology and focuses on both basic science and clinical research in the field. In the past 22 years, they have developed a niche area investigating the etiology and pathogenesis of Giant Cell Tumor of Bone (GCTB), and over 90 peer-reviewed journal articles have been published.
 |
|
|
Dr. WONG Kwok-chuen |
Research Background and Direction
GCTB is a nonmalignant, primary bone tumor which contributes about 20% of all skeletal neoplasms in Chinese population. It is typically found at the epiphyseal ends of long bones & its prime radiological characteristic is the presence of large expansile osteolytic lesions. GCTB is well known for its potential to recur following treatment, local recurrence rates of 18% to 50% have been reported.
In basic research, they have investigated the molecular events of histogenesis and biological behavior of GCTB, and the transcriptional regulation of RANKL promoter in this tumor. Moreover, they have also studied the molecular mechanisms for different drugs applying on GCTB treatments, such as nitrogen-containing bisphosphonates, prenyl transferase inhibitors, and denosumab. Recently, differential gene expression of the neoplastic GCTB stromal cells have been studied with the Next Generation Sequencing technique. 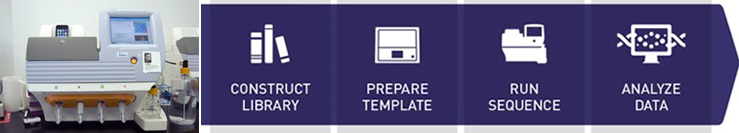 In clinical studies, they have done the pioneering work on computer assisted tumor surgery, to establish a unique computer-assisted workflow in musculoskeletal tumor surgery. In addition, they have used tumor prostheses in limb salvage surgery for patients with bone tumors and surgical techniques to insert complex custom tumor prostheses, to develop the Asian modification of tumor prostheses for Chinese population. They have received a number of both local and international awards in this field.
On-going Research / Projects
| Project Title |
Funding Agency |
Award Year |
| Computer Adaptive Testing Promotes Mastery Learning |
Teaching Development Grant,
CUHK |
2017 |
| Provision for Development and Maintenance Service of Web-based Training Courseware for HA Central Intern Orientation Program |
Hospital Authority |
2015 |
| Differentiation therapy of Giant Cell Tumor of Bone using the U.S. Food and Drug Administration (FDA)-approved drugs, Parathyroid Hormone, Rapamycin and Simvastatin |
CUHK Direct Grant |
2015 |
| Provision of Development of Web-based Training Courseware for Hospital Authority Central Orientation Program |
Hospital Authority |
2013 |
| The Investigation of potential anti-tumor effects of Denosumab on GCT of bone |
CUHK Direct Grant |
2013 |
| E&M-based Video Vignettes for Upper Extremity Neurological Examination |
Courseware Development Grant 2012-13 |
2013 |
| Implementing MEDLOG & E-portfolio to Improve Student Engagements in Self-Initiated Clinical Encounters and Participation in Practical Procedures |
Teaching Development Grant,
CUHK |
2013 |
| Determining the Precision and Accuracy of Computer Assisted Bone Tumor Surgery: A Study Comparing Computer Navigation with Patient Specific Cutting Guides in Cadavers |
General Research Fund,
Research Grants Council,
Hong Kong |
2012 |
| Treatment of Giant Cell Tumor of Bone by the Combination of Nitrogen-Bisphosphonates and Phenyl Transferase Inhibitors: An in vivo study |
General Research Fund,
Research Grants Council,
Hong Kong |
2012 |
Research Impacts
Awards
| • |
Hospital Authority Outstanding Team Award 2014 (Paediatric sarcoma as part of paediatric oncology service in CCC). |
| • |
"Navigation assisted Bone tumor surgery" was chosen as one of the medical advancement at 30th Anniversary of Prince of Wales Hospital in 2014. |
| • |
Use of Computer navigation in bone cancer surgery was chosen by Hong Kong government as one of the Advanced Healthcare in Hong Kong (2011-2013). |
| • |
CORR multimedia article award in 2012. |
| • |
The work on "Bone tumor surgery with computer navigation" was chosen as one of the two leaders (the other is liver transplants from HKU) in medical science and a pioneering member of international medical fraternity in applied research and practice in Hong Kong. It is published by Information Services Department – Hong Kong Special Administrative Region (HKSAR) Government (2008-2011). |
| • |
Poster prizes at ISOLS meeting in 2007 and 2011. |
| • |
The work on "Bone tumor surgery with computer navigation" was also chosen as one of the ten academic and research achievements at the 45th anniversary of CUHK in 2009. |
| • |
Best Clinical Paper award at CAOS-international meeting in 2008. |
Press Releases, News Articles
Selected Publications
| 1. |
Wong KC, Niu X, Xu H, Li Y, Kumta S. Computer Navigation in Orthopaedic Tumour Surgery. Adv Exp Med Biol. 2018;1093:315-326. |
| 2. |
Lau CP, Kwok JS, Tsui JC, Huang L, Yang KY, Tsui SK, Kumta SM. Genome-Wide Transcriptome Profiling of the Neoplastic Giant Cell Tumor of Bone Stromal Cells by RNA Sequencing. J Cell Biochem. 2017 Jun;118(6):1349-1360. |
| 3. |
Chen S, Lau P, Lei M, Peng J, Tang T, Wang X, Qin L, Kumta SM. Segmental composite porous scaffolds with either osteogenesis or anti-bone resorption properties tested in a rabbit ulna defect model. J Tissue Eng Regen Med. 2017 Jan;11(1):34-43. |
| 4. |
Wong KC, Sze KY, Wong IO, Wong CM, Kumta SM. Patient-specific instrument can achieve same accuracy with less resection time than navigation assistance in periacetabular pelvic tumor surgery: a cadaveric study. Int J Comput Assist Radiol Surg. 2016 Feb;11(2):307-16. |
| 5. |
Lau CP, Wong KC, Huang L, Li G, Tsui SK, Kumta SM. A mouse model of luciferase-transfected stromal cells of giant cell tumor of bone. Connect Tissue Res. 2015 Nov;56(6):493-503. |
| 6. |
Wong KC, Kumta SM. Use of Computer Navigation in Orthopedic Oncology. Curr Surg Rep. 2014 Feb 22;2:47. eCollection 2014. Review. |
| 7. |
Lau CP, Huang L, Wong KC, Kumta SM. Comparison of the anti-tumor effects of denosumab and zoledronic acid on the neoplastic stromal cells of giant cell tumor of bone. Connect Tissue Res. 2013;54(6):439-49. |
| 8. |
Wong KC, Kumta SM. Computer-assisted tumor surgery in malignant bone tumors. Clin Orthop Relat Res. 2013 Mar;471(3):750-61. |
| 9. |
Lau CP, Ng PK, Li MS, Tsui SK, Huang L, Kumta SM. p63 regulates cell proliferation and cell cycle progression‑associated genes in stromal cells of giant cell tumor of the bone. Int J Oncol. 2013 Feb;42(2):437-43. |
| 10. |
Wong KC, Kumta SM, Sze KY, Wong CM. Use of a patient-specific CAD/CAM surgical jig in extremity bone tumor resection and custom prosthetic reconstruction. Comput Aided Surg. 2012;17(6):284-93. |
| 11. |
Tang T, Zhang G, Lau CP, Zheng LZ, Xie XH, Wang XL, Wang XH, He K, Patrick Y, Qin L, Kumta SM. Effect of water-soluble P-chitosan and S-chitosan on human primary osteoblasts and giant cell tumor of bone stromal cells. Biomed Mater. 2011 Feb;6(1):015004. |
| 12. |
Lau CP, Huang L, Tsui SK, Ng PK, Leung PY, Kumta SM. Pamidronate, farnesyl transferase, and geranylgeranyl transferase-I inhibitors affects cell proliferation, apoptosis, and OPG/RANKL mRNA expression in stromal cells of giant cell tumor of bone. J Orthop Res. 2011 Mar;29(3):403-13. |
| 13. |
Wong KC, Kumta SM, Leung KS, Ng KW, Ng EW, Lee KS. Integration of CAD/CAM planning into computer assisted orthopaedic surgery. Comput Aided Surg. 2010;15(4-6):65-74. |
| 14. |
Wong KC, Kumta SM, Tse LF, Ng EW, Lee KS. Navigation Endoscopic Assisted Tumor (NEAT) surgery for benign bone tumors of the extremities. Comput Aided Surg. 2010;15(1-3):32-9. |
| 15. |
Ng PK, Tsui SK, Lau CP, Wong CH, Wong WH, Huang L, Kumta SM. CCAAT/enhancer binding protein beta is up-regulated in giant cell tumor of bone and regulates RANKL expression. J Cell Biochem. 2010 May 15;110(2):438-46. |
| 16. |
Tse LF, Wong KC, Kumta SM, Huang L, Chow TC, Griffith JF. Bisphosphonates reduce local recurrence in extremity giant cell tumor of bone: a case-control study. Bone. 2008 Jan;42(1):68-73. |
| 17. |
Wong KC, Kumta SM, Chiu KH, Cheung KW, Leung KS, Unwin P, Wong MC. Computer assisted pelvic tumor resection and reconstruction with a custom-made prosthesis using an innovative adaptation and its validation. Comput Aided Surg. 2007 Jul;12(4):225-32. |
| 18. |
Wong KC, Kumta SM, Chiu KH, Antonio GE, Unwin P, Leung KS. Precision tumour resection and reconstruction using image-guided computer navigation. J Bone Joint Surg Br. 2007 Jul;89(7):943-7. |
|